Immune-mediated thrombotic thrombocytopenic purpura (iTTP) results from autoantibody-mediated severe deficiency of ADAMTS13, the Von Willebrand factor (VWF)-cleaving protease. In this context, ultra-large VWF multimers accumulate in the circulation, leading to increased platelet clumping, with subsequent severe thrombocytopenia, microangiopathic hemolytic anemia and multiorgan failure. The anti-VWF nanobody caplacizumab is licensed for adults with iTTP. Prospective controlled trials and national real-world studies have provided evidence that caplacizumab improved outcome of the acute phase of the disease. However, whether caplacizumab decreases mortality, and the optimal timing of caplacizumab initiation, remain to be determined. To address these questions, an international survey, the Capla 500+ project, has been conducted.
An academic call for observations involving experienced teams from 10 worldwide countries recruited 942 adult patients treated with a regimen of daily therapeutic plasma exchange (TPE), caplacizumab and immunosuppression with corticosteroids ± rituximab (caplacizumab group). Cases were compared to historic controls (control group) randomly selected from 2015 to 2018 by 4 teams in a 2:1 ratio (N=495), treated with TPE and immunosuppression. Primary outcome was 3-month survival post-first TPE. Key secondary outcomes were refractoriness and exacerbations, time to clinical response, number of TPE to achieve clinical response, time to ADAMTS13 activity recovery ≥20%, and caplacizumab-related adverse events.
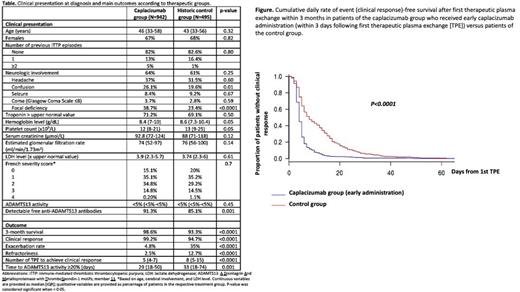
Clinical presentation and severity were comparable between groups ( Table). All patients received TPE in both caplacizumab and control groups, in association with corticosteroids (99% and 93%, respectively), and rituximab (92% and 71%, respectively) frontline or as salvage therapy. Caplacizumab was started within 3 days (715 patients), or delayed by≥4 days from first TPE (218 patients); for those with delayed initiation, caplacizumab was added for management of exacerbation or refractoriness (63 cases) or a slow improvement to TPE/immunosuppression (155 cases). The 3-month survival post-first TPE in the caplacizumab group was 98.6% vs 93.3% in the control group (p<0.0001). Failure to achieve clinical response was 5-times less likely in the caplacizumab group as compared to the control group (95% confidence interval, 0.1-0.37, p<0.0001). Deaths in the caplacizumab group occurred after a median of 4.5 days (interquartile range [IQR], 3-5), mostly due to uncontrolled iTTP. Patients receiving caplacizumab experienced less refractoriness and exacerbations, and required less TPE to achieve clinical remission than controls (p<0.0001 for all), regardless of the use of rituximab. Forty-six patients experienced an exacerbation following caplacizumab interruption while ADAMTS13 activity was still undetectable. Time to ADAMTS13 activity ≥20% was shorter in the caplacizumab group (p=0.01) ( Table), where rituximab was more systematically used. In patients with delayed caplacizumab initiation, clinical response was obtained after a median of 4 days (IQR, 2-8) following caplacizumab introduction. This result was comparable to the time to clinical response obtained in patients who initiated caplacizumab within 3 days of the first TPE (median, 4 days [IQR, 3-6], p=0.8). In patients with early caplacizumab initiation, unfavorable outcomes were particularly infrequent (death, 1%; refractoriness, 1.1%; exacerbations, 5.3%),andtime to clinical response in survivors was half the time compared to control group survivors (p<0.0001) ( Figure). Caplacizumab-related adverse events occurred in 220 patients (23%). They consisted of major bleeding (N=19, 2.2%), including: digestive tract bleeding (N=8), intracranial hemorrhage, severe central venous catheter insertion bleeding, metrorrhagia (N=2 cases each). Clinically relevant non-major bleeding (N=34, 3.7%), non-clinically relevant non-major bleeding (N=114, 14%), and inflammatory reaction at the injection site (N=35, 4.5%) were also reported.
This unprecedented, international academic effort on such a rare disease provides convincing evidence that caplacizumab added to TPE and immunosuppression prevents unfavorable outcomes during the acute phase of iTTP, including mortality, and alleviates the burden of care at the potential expense of rare, major bleeding events.
Disclosures
Coppo:SANOFI: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; TAKEDA: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; ALEXION: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Benhamou:SANOFI: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Voelker:Alexion: Honoraria; Sanofi-Genzyme: Honoraria; Bayer: Honoraria; AstraZeneca: Honoraria; GC Biopharma: Honoraria. Brinkkoetter:AstraZeneca: Honoraria; Bayer: Honoraria; Vifor CSL: Honoraria; Travere: Honoraria; Novartis: Honoraria; Alexion: Honoraria; Roche: Honoraria; Sanofi-Genzyme: Honoraria, Research Funding. Kühne:Alexion: Honoraria. Knoebl:Technoclone: Honoraria; Alexion: Honoraria; Biotest: Honoraria; CSL Behring: Honoraria; Roche: Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; NovoNordisc: Honoraria, Research Funding; Ablynx/SOBI: Honoraria, Research Funding. De La Rubia:Janssen: Honoraria, Speakers Bureau; Pfizer: Speakers Bureau; Sanofi: Speakers Bureau; Takeda: Research Funding; Menarini: Honoraria; GSK: Honoraria, Research Funding, Speakers Bureau; BMS: Honoraria; Oncopharm: Honoraria. Chaturvedi:Alexion: Consultancy, Other: Advisory board participation; Sanofi Genzyme: Consultancy; Takeda: Other: Advisory board participation; Sobi: Honoraria; Sanofi: Other: Advisory board participation. Masias:Sanofi: Consultancy; Takeda: Consultancy; Argenx: Consultancy; Rigel: Consultancy. Zheng:Apollo: Consultancy, Honoraria; GC Biopharma: Consultancy, Honoraria; Clotsolution: Other: Co-founder; Sanofi: Consultancy, Honoraria; Stago: Consultancy, Honoraria; TAKEDA: Consultancy, Honoraria. Patriquin:TAKEDA: Consultancy, Honoraria. Veyradier:TAKEDA: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; SANOFI: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Sakai:Takeda: Research Funding. Matsumoto:Chugai Pharmaceutical: Research Funding; Alexion Pharma: Consultancy, Research Funding, Speakers Bureau; Takeda: Consultancy, Speakers Bureau; Asahikasei Pharma: Research Funding, Speakers Bureau; Sanofi: Consultancy, Research Funding, Speakers Bureau. Peyvandi:Biomarin: Membership on an entity's Board of Directors or advisory committees; Sobi: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; CSL Behring: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Spark: Speakers Bureau; Takeda: Speakers Bureau. Dutt:SANOFI: Consultancy, Honoraria. Cataland:Takeda: Consultancy; Sanofi: Consultancy. Scully:Takeda: Honoraria, Research Funding, Speakers Bureau; Alexion: Research Funding; Octopharma: Speakers Bureau; Sanofi: Honoraria, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal